By Kadee Klafka, RN, Cardiac Intensive Care, IU Health Ball Memorial Hospital—
From a nurse’s eyes.
I’ve been surrounded by a lot of different views of the global pandemic. I am entirely full of anger; I’ll do my best to keep all the emotions I’m personally dealing with out of these experiences and thoughts I’m about to share.
In the beginning of the pandemic, we were all scared. We didn’t know what this virus was. We didn’t know how it would affect our lives. I vividly remember the first case we thought we had in our ICU because the chest x-ray read “ground glass opacities.” We didn’t know how to protect ourselves. But time went on. Research was done as quickly as possible to figure out if it was spread via aerosolized particles, droplets, or if it was airborne. Protocols changed quickly within the hospital. Wear a mask, wear an N95… now add eye protection.
Now you don’t need an N95 unless your patient is on the bipap or ventilator. Oh but now you only need an N95 if your ventilated patient has gotten an aerosolized treatment or their circuit has broken within the last 69 minutes. Things changed so rapidly because we were learning and gaining new information so quickly, while also trying to preserve resources- we weren’t prepared for this.
Now we’ve been going through this for nearly 19 months. We’ve got more N95s, more PPE, and by December 2020, we were vaccinating healthcare workers, first responders, and high risk patients. Now, you’re information overloaded. Overwhelmed by numbers, statistics, graphics of how many patients are in each hospital, and how many are covid and unvaccinated. You watch the news, you see restrictions implemented in attempts to keep others from being infected.
Some see these numbers and graphics showing covid data and think we’re “trying to push an agenda.” But there’s so much more you don’t see. There’s such a limited view into the hospitals.
You don’t see nurses sharing their stories, because we protect our patient’s privacy. But more and more, I’m realizing it might be our experiences that speak louder than numbers.
We do everything we can for our patients. Many patients come in short of breath, with low oxygen readings, we put them on oxygen, start medications including antivirals and steroids. But then that oxygen and medication isn’t enough. We keep turning the oxygen up, and up, and up, until we get to the point they have to wear a mask that forces air into their lungs. Soon, even that is not enough. They need to be intubated.
So Emily, RN, our charge nurse for the day, calls their family and tells them we can’t keep their oxygen up and it’s time to be intubated. Caroline, RN hurries to the med room to grab medications to sedate and paralyze them so that our pulmonologist can intubate safely and quickly. Jessica, our respiratory therapist, grabs her RT friend Salina and they wheel in the ventilator.
Everyone dons their PPE and is ready at the patient’s bedside. Caroline pushes meds, RT handles the airway and tools necessary for intubation. Our pulmonologist intubates them. Angie, our rapid response nurse, records the events from just outside the room with the phone on speaker so she can hear inside.
After successful intubation, we put in a foley catheter, a nasogastric tube (tube in your nose or mouth down to your stomach so we can give you medications and nutrition). We get x-rays and labs. We start continuous sedation so the patient can comfortably tolerate the tube in their mouth that is anchored by a balloon in the trachea. The ventilator settings are immediately increased. When 100% oxygen isn’t keeping their oxygen levels up, we increase the pressure so that their lungs are kept open and hope for better oxygenation. Emily and Caroline hold their hand and watch the monitor hoping for their oxygen to get above 88%.
When it doesn’t, the pulmonologist tells us to start the paralytic medication and flip them onto their stomach and hope that gravity helps recruit more of their lungs to oxygenate. Prone therapy is working and we are so glad to get their oxygen up into the 90s. We do this for four or five days. They’re not getting better and their blood pressure starts to drop. We start medications for this. It’s not working… their kidneys start to shut down, we start continuous dialysis.
Steve Lindell interview with hospital president Dr. Jeff Bird on the virus crisis at Ball Hospital.
Family comes and hangs onto every piece of hope we can offer. Each 5% decrease in the patient’s oxygen needs is a win. But it’s becoming more and more clear they won’t make it. We talk to their family- we talk about quality of life and what the patient would’ve wanted if we’d exhausted every life saving option. Their family knows they won’t want to live like this; they’ve come to realize they won’t get better. So a decision is made to turn our care from aggressive treatment to making the patient as comfortable as possible in their last hours.
Just a couple days ago, Emmy found herself taking care of Henry (name changed to protect privacy). Covid positive, unvaccinated just because he hadn’t had the time. On the ventilator, 100% oxygen. We’d tried everything. Prone, antivirals, steroids- all of it. But it was obvious he wasn’t going to recover from this. So his family came in and said their goodbyes and made the decision to make him comfortable. The family was appreciative of our care for Henry, but didn’t want to stay with him as he passed away. Respiratory therapy extubated him.
Emmy, Emily, and I did what we could to make him comfortable with the morphine and ativan. Emmy held one hand, Emily had the other. I messaged the doctor back and forth to make sure we had what we needed for Henry as he took his last breaths. We stood at Henry’s bedside for minutes. We watched him take a few gasping breaths, we held his hand and turned his pillows. We made sure he wasn’t in pain. Emily and I watched tears slide down Emmy’s face and into her N95. Five minutes later, the monitor read asystole. No heartbeat. No breathing.

Meridian Health Services and Urban Light Church partnered to bring Johnson & Johnson COVID-19 vaccines to area residents. Photo by Lorri Markum
Henry was one of too many. Just this yesterday, we lost our patient Penny. Over the months, we’ve lost Gary, Joe, Tommy, Susan, Paulette, Chris, Carry, Richard, and so many more. (Names changed to protect privacy.)
People come to their own conclusions looking at the numbers and survival rates and brush it off. It’s not likely to affect them, so they don’t think too hard about it. Or, maybe it is too much information to process. But from my point of view, I see Henry, Susan, and Joe who didn’t deserve this.
We are so tired. Exhausted. Mentally and emotionally undone…. because we don’t see numbers. I see my patients and their family members. I see the grief and share it with them. Now, there’s a vaccine, which makes this virus preventable and/or so much more mild that patients wouldn’t need the hospital if they did get it. Some of my closest family members continue to decline to get the vaccine and I’m so frustrated and tired and angry.
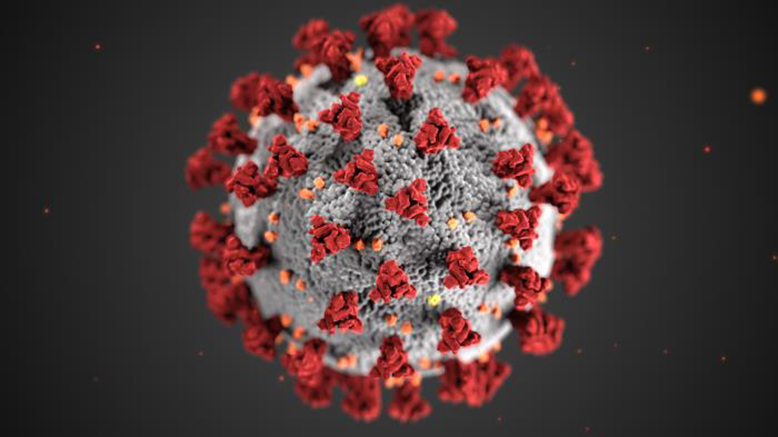
This illustration, created at the Centers for Disease Control and Prevention (CDC), reveals ultrastructural morphology exhibited by coronaviruses. Note the spikes that adorn the outer surface of the virus, which impart the look of a corona surrounding the virion.
I am a nurse and I will take care of my patients and be the best advocate no matter who you are or any choices you’ve made… but there’s a way to help, and that way is masking and getting the vaccine. Help us so that maybe we won’t be the one to hold your loved ones hand while they pass away. It’s an honor to be that person for these patients, but right now, it doesn’t have to be this way.
And maybe it’s not only my stories that the community needs to hear. They need to hear the stories of Kat, Sarah, Kellen, Crystal, Paige, Daniela, Katie, Kelsie, Jamie, Haley, Taylor, Sheryl, Natalie, Bre, Matt, and so many more taking care of our community during covid.
Emmy is a CIC nurse taking care of covid patients every day.
“I have participated in a minimum of 2 deaths per day in the last nine days. And one day there were five. In some of these cases, it’s not the doctor having the conversations with the families, it’s me. And somehow I’m the last person they’ll ever speak to while also being the person to listen to their heart beat the last time and tell their wife or husband “they’re gone.” Somehow I’m crying and grieving a person I never knew. Shouting in a dirty utility room. Putting myself in time out so I can walk into the next room while others live comfortably unaware.”
Emmy, CICU RN—Conversations we have with our patients:
“Hi, my name is Emily, I’m one of the nurses caring for you. Here in a minute there are going to be a lot of people coming to your room. Your oxygen is not staying high enough anymore.”
“No honey, there’s nothing more you can do.”
“If we wait any longer, it will become an emergency and it’s better to do it now while you’re safe.”
“I’m so sorry, we can’t wait for your wife to come. There is no more time.”
“I can’t say how long you will need this.”
“I promise to do everything I can.”
“I’ll tell them you love them.”
And repeat.
Published by MuncieJournal.com with permission from IU Health Ball Memorial Hospital and Kadee Klafka, RN, Cardiac Intensive Care.



